News
News
Catch up on the latest industry news and foot health tips below.

By Asha Curry
•
February 4, 2025
At MJ Taranto, we understand undergoing surgery can feel overwhelming, and we want you to know that at our clinic, your recovery and well-being are our top priorities. Our team is passionate about providing the best experience for every patient, and we go above and beyond to ensure you feel supported every step of the way. What Makes Our Care Unique? Personalised Attention: After your surgery, you won’t just see a nurse—you will see your surgeon for all your post-operative care. This means that every redress, check-up, and follow-up is handled by the person who knows your case best: your surgeon. Direct Access: We believe in open communication. If you have concerns or questions during your recovery, you can contact us personally, even outside of clinic hours. We’re here for you when you need us most. Dedicated Administrative Support: Our clinic has staff members who specialise in supporting our surgical patients. From the moment you decide to proceed with surgery, our dedicated administrative team will guide you through the entire process. They will help you prepare for surgery, answer any questions you may have, and ensure you feel confident and informed every step of the way. Full Investment in Your Recovery: Your recovery is a journey, and we are fully committed to helping you every step of the way. From pre-operative education to detailed recovery plans, we ensure you’re well-informed and confident in your progress. What to Expect During Recovery While every patient’s recovery timeline is unique, here are some general guidelines to help you plan: Initial Healing: The first few weeks are focused on wound healing and managing swelling. We will guide you on how to care for your surgical site and keep you comfortable. Gradual Return to Activities: Over the next few months, we’ll work together to help you safely return to your normal activities. This timeline will be tailored to your specific surgery and progress. Long-Term Recovery: Full recovery from most surgeries can take 12 to 18 months. During this time, we will monitor your progress and address any concerns that arise. Patience is key, but rest assured, we’re with you for the long haul. Pre-Operative and Post-Operative Communication Communication is at the heart of what we do. Before your surgery, we will provide you with detailed information about what to expect, including a recovery timeline. Knowing what lies ahead can make a big difference in how you approach your recovery. After your surgery, our lines of communication remain open. Whether it’s a question about your recovery, guidance on wound care, or simply reassurance, you can count on us to be available and responsive. Our Commitment to Excellence At our clinic, you’re not just another patient—you’re part of our care family. From the moment you walk through our doors to the final stages of your recovery, we are dedicated to providing one-on-one care that’s second to none. Your health, comfort, and satisfaction are our top priorities.

By Asha Curry
•
October 10, 2024
Let’s take a moment to talk about something that’s all too familiar for many of us: bunions. You know, those pesky bumps that form on the side of your big toe and seem to make wearing shoes a daily battle? If you’ve been tiptoeing around the subject of bunions, it’s time to shed some light on what they are and how we can help you take the next step towards relief. Mary, a vibrant 65-year-old who loves gardening and taking long walks, started noticing a sharp pain in her foot. At first, she shrugged it off, thinking it was just part of getting older. But as the months went by, the pain worsened, and she noticed a bony bump forming on the side of her big toe. She’d had a small prominence here for a few years but it had never really bothered her before. Eventually, she found herself avoiding her beloved walks and spending more time sitting down. And when she did walk, she felt unsteady, almost like she could lose her balance at any moment. After a bit of research, Mary discovered her pain was due to a bunion. Like many of us, she tried non-surgical options first—wider and deeper shoes, protective padding, and even a few over-the-counter pain relievers. While these provided temporary comfort, they didn’t solve the problem. The bump continued to grow, and Mary’s fear of falling increased. Here’s the thing: bunions can become more than just a cosmetic issue or a source of discomfort. As they worsen, they can change the way you walk and increase your risk of falls, especially as we age. This is where surgical correction comes into play. For Mary, choosing bunion surgery meant more than just addressing the bump on the side of her foot; it was about reclaiming her mobility and independence. The procedure relieved her pain, corrected her toe’s alignment, and allowed her to get back to her active lifestyle without the constant worry of tripping or falling. Bunion surgery isn’t a one-size-fits-all solution but for many, it can significantly improve quality of life. Our podiatric surgeons, Michael and Julie Taranto, are experts in assessing whether surgery is the right choice for you. They’re here to help you understand your options, whether it’s opting for a non-surgical approach or deciding that surgery is the best path forward. So, if you or a loved one are dealing with bunions and the pain and balance issues that often come with them, don’t let it sideline you any longer. Take the first step towards comfort and confidence by scheduling an appointment with Michael or Juile Taranto today. We’re here to help you walk with ease again! Surgery is not without its risks, but it’s worth getting all the information so you can make an informed decision. We pride ourselves on being able to provide availability for our patients, with same-day appointments usually available.

By Asha Curry
•
August 6, 2024
For as long as she could remember, Amanda had been living an active, fulfilling life. She enjoyed spending time with friends, going on weekend hikes, and even the simple pleasure of walking her dog in the park. But twelve months ago, a nagging pain in her heel began to rob her of her joy. It started as a dull ache, but soon every step felt like walking on broken glass. The diagnosis? Plantar fasciitis. To make matters worse, she was also experiencing symptoms of tarsal tunnel syndrome. Amanda threw everything she had at the pain. She tried resting, icing, and changing her footwear. She invested in custom orthotics, followed rigorous exercise routines, and took anti-inflammatories regularly. She underwent shock wave therapy sessions, hopeful that each session would be the one to make a difference. Cortisone injections offered brief relief, but the pain always came back, often worse than before. Her quality of life declined rapidly, making standing for long periods at work unbearable. Social outings became rare, as she dreaded the inevitable pain, with friends commenting they could see the pain in her face. It permeated every aspect of her life, turning even the simplest activities into ordeals. She missed out on hikes, family gatherings, and even trips to the grocery store became daunting. One particularly painful morning, as Amanda struggled to make it from her bed to the bathroom, she realised she couldn't go on like this. It was time for a different approach. She booked an appointment with Michael Taranto, one of our Podiatric Surgeons, ready to discuss surgical options. At the consultation, Michael listened to Amanda’s story with empathy and understanding and together they reviewed her history and explored surgical options. Michael assured Amanda that her investments in orthotics weren't wasted—they would remain an important part of her treatment regime even after surgery. Amanda felt a glimmer of hope for the first time in months, and though she wasn’t looking forward to the recovery, she knew the time had come for surgery. Michael explained the realistic expectations around pain reduction and the potential to regain quality of life. Amanda's story is a reminder that sometimes, despite our best efforts with non-surgical measures, seeking the expertise of a Podiatric Surgeon can be the turning point. If you, like Amanda, have been struggling with persistent heel pain and have exhausted all other options, it might be time to take the next step. Come see one of our Podiatric Surgeons, Michael Taranto or Julie Taranto, to discuss your options and start enjoying the simple things in life again. Your future self will thank you.

By Asha Curry
•
June 6, 2024
Does your ankle feel like it’s locking, catching or giving way at times? Unstable ankles are very common and are not just a result of repeated ankle sprains, although they certainly don’t help! The ankle is made up of bones, joints, cartilage, ligaments, a soft tissue envelope called the capsule, and the fascia and retinaculum that help to hold the ankle together. Repetitive stress on the ankle, whether through wear and tear or an ankle sprain or fracture, can cause ongoing instability in the ankle. Cartilage damage, loose bony fragments, pinched scar tissue in the ankle joint, or ruptured or stretched ligaments can all contribute to instability, pain, and swelling. Whilst there are conservative options for the treatment of symptoms of ankle instability, such as ankle braces, supportive footwear, targeted exercises, and orthotics, there are instances where instability and pain will persist. In these cases, surgery can be undertaken to reconstruct the ankle ligaments and remove any floating bone or damaged cartilage. The recovery from ankle reconstruction surgery is quite lengthy and involves physiotherapy as part of the rehabilitation process. If you have symptoms associated with ankle instability, come in and see one of our Podiatric Surgeons who will be able to assess and discuss your options in more detail. Call 9250 1676 or book through our website.

April 12, 2024
Not Just Plantar Heel Pain The long Perth summer goes hand in hand with wearing thongs and being down at the beach. It’s important to be mindful that this extended period in unsupportive shoes can exacerbate underlying or existing issues in the plantar fascia (band beneath the arch of the foot), or trigger new symptoms in the arch and heel. You might have heard about plantar fasciitis, which is quite common and can be a real pain in the heel (literally), but did you know that there's more to heel pain than just that? Let's talk about it. Plantar Heel Pain 101 Plantar heel pain is any kind of discomfort or ache you feel in your heel area. While plantar fasciitis is a common cause, there are other culprits too. One of them is something called tarsal tunnel syndrome. Tarsal Tunnel Syndrome: A Sneaky Troublemaker Tarsal tunnel syndrome is similar to carpal tunnel syndrome, which occurs in the wrist. Imagine a tunnel in your foot where important nerves and blood vessels pass through. If that tunnel gets squeezed or compressed, you've got yourself tarsal tunnel syndrome. It can feel a lot like plantar fasciitis, but it's a whole different ball game. With tarsal tunnel syndrome, you might experience tingling, burning, or shooting pains that travel from your heel down to your toes or in the other direction too. Sometimes it can feel like electric shocks zapping your foot. What’s Going on Inside? So, why does this happen? There are a few common possibilities. It could be due to an unusual foot structure or an injury or past trauma, like a sprained ankle. Other times it’s caused by pressure from blood vessels or other soft tissue structures in the area. And sometimes it's just bad luck and your nerves get irritated for no apparent reason. Treatment Options: Finding Relief Okay, enough with the doom and gloom. Let's talk about what we can do to ease the pain. For starters, there are some simple tricks you can try at home: · Rest: Give your feet a break. Avoid activities that make the pain worse. · Ice: Apply an ice pack to your heel for about 15 minutes a few times a day to reduce inflammation, or roll your foot on a frozen water bottle to give the effect of ice massage. · Stretching: Gentle stretches of the calf and foot can help loosen up tight muscles and ease tension. If these DIY remedies aren't cutting it, it might be time to see a healthcare professional. Our podiatrists can assess you and may recommend: · Medical Imaging: Diagnosis is key in achieving optimal results. · Orthotics: Custom-made shoe inserts can provide extra support and cushioning for your feet. · Physiotherapy: Working with a physio can help strengthen your muscles and improve your range of motion. · Medication: Pain relievers or anti-inflammatories might offer some relief. · Shockwave Therapy: High-energy acoustic waves are delivered into the tissue to stimulate healing. · Injection Therapy: such as guided corticosteroids or PRP (platelet-rich plasma) Surgical Option: Last Resort Surgery to decompress (relieve tension in the tarsal tunnel) is usually the last resort when all other treatment options have been unsuccessful. If your symptoms are severe and impacting your daily life, our Podiatric Surgeons Julie Taranto or Michael Taranto may recommend surgical decompression of the tarsal tunnel. It sounds scary, but it's often very effective in relieving pain and restoring function.

February 8, 2024
Hammer Toe Correction Surgery Hammer toes, a common foot deformity where the toes bend unnaturally at the joints, causing pain and discomfort, has seen significant advancements in corrective surgeries. As a trusted provider of podiatric surgery in Australia, our surgeons remain committed to staying at the forefront of these developments to ensure optimal patient outcomes. Understanding Hammer Toe Hammer toes typically result from an imbalance in the muscles, tendons, or ligaments that hold the toe straight. Over time, this deformity can become rigid and painful, hindering daily activities. Indications for Surgery While conservative treatments like proper footwear and orthotics may alleviate mild symptoms, surgical intervention becomes essential for severe cases that impede normal function. This may include persistent pain, difficulty walking, or the development of friction lesions or open sores. Surgery Surgical techniques are individually tailored for each patient, with the majority of surgery being day-case surgery, that is, in and out on the same day and being able to weight bear immediately. The aim of surgery is to perform targeted correction of the hammer toe deformity while preserving function. Patient-Centric Care Our surgeons tailor each intervention to the unique needs of the patient. From pre-operative evaluations to post-operative care, a comprehensive approach ensures the best possible results. We prioritise patient education, fostering a deep understanding of the procedure and expectations. Recovery and Rehabilitation Advancements in surgical techniques contribute to quicker recovery times and improved outcomes. Following surgery, patients are guided through rehabilitation protocols to enhance strength, flexibility, and overall foot function. If you or someone you know is struggling with hammer toe deformities, the surgeons at MJ Taranto Foot and Ankle Podiatric Surgeons are here to provide expert guidance and tailored solutions. Contact the skilled surgeons at MJ Taranto Foot & Ankle Podiatric Surgeons today for a consultation on 9250 1676 or click the link to book online.
By Asha Curry
•
November 6, 2023
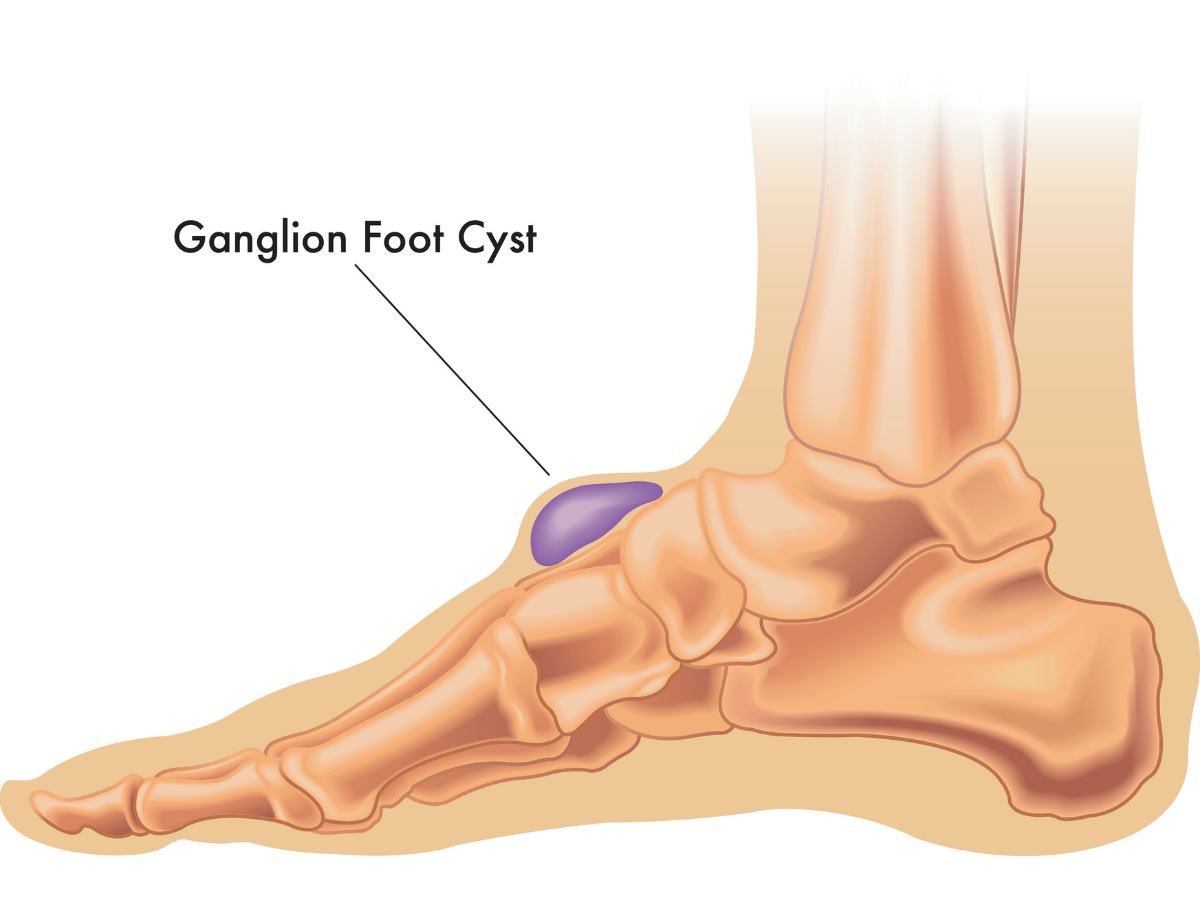
Surgical Management of Ganglion Cysts in the Foot: Regaining Comfort & Mobility Ganglion cysts, fluid-filled sacs that often form around tendons or joints in the foot, can be a source of discomfort and uncertainty for many individuals, causing pain, stiffness, and reduced mobility. In Australia, podiatric surgeons are well-versed in the surgical management of ganglion cysts, offering patients a path to relief and improved foot function. Understanding Ganglion Cysts: Ganglion cysts are non-cancerous lumps that typically develop near the joints or tendons of the foot. While the exact cause is not always clear, they are often associated with repetitive stress or overuse of the affected area. These cysts can vary in size, and their presence may lead to discomfort when walking, exercising, or simply standing for extended periods. When is Surgical Management Considered? Surgical intervention becomes an option when conservative treatments, such as rest, aspiration (draining the cyst with a needle), or corticosteroid injections, do not provide lasting relief, or when the cyst returns after aspiration. Surgery may also be recommended if the cyst affects joint function, leads to instability, or causes significant pain. The Surgical Procedure: Ganglion cyst surgery aims to remove the cyst and its adjacent tissue. The procedure typically involves making an incision over the cyst and carefully excising it. In some cases, the surgeon may also address any underlying joint or tendon issues contributing to the cyst's development. Recovery and Rehabilitation: Recovery time varies depending on the specific procedure, but patients can often weight bear immediately following the procedure and resume normal function within a few weeks. Post-operative physical therapy may be recommended to aid in restoring strength, flexibility, and overall foot function. If you're experiencing the discomfort of a ganglion cyst in your foot, don't hesitate to consult with a qualified podiatric surgeon at MJ Taranto Foot and Ankle Podiatric Surgeons to explore the options available to help you regain comfort, mobility, and improved quality of life.

By Asha Curry
•
September 5, 2023
Are you familiar with the term Podiatric Surgeon, but unsure of what it entails? This month, we’re diving into the history of the profession in Australia, and shedding light on the role Podiatric Surgeons can play in treating foot and ankle conditions. Podiatric Surgery has been a profession in Australia since 1976 and is now recognised as a specialty surgical profession by the Australian Health Practitioner Regulation Agency (AHPRA). Podiatric Surgeons make up less than 1% of registered Podiatrists practising in Australia. They're unique Podiatrists qualified to diagnose and treat disorders of the foot, ankle, and related structures using medical and surgical methods. To become a Podiatric Surgeon, they must undergo extensive postgraduate training and education, dedicating themselves to many years of study, research, and practice to investigate and master medical and surgical therapeutics of the foot and ankle. So, essentially, they're Podiatrists who have levelled up. Podiatric Surgeons can treat a wide range of conditions such as structural deformities, heel pain and nerve conditions, tendon and soft tissue problems, foot and ankle arthritis, skin and nail conditions, birth defects of the foot, and trauma injuries (fractures and dislocations). They will discuss the best treatment options, both surgical and non-surgical (not everyone needs foot surgery), with their patients to help them select a plan that balances their needs and expectations with delivering the best outcome. Podiatric Surgeons have a long history of safe practice in Australia, operating in private hospitals and adhering to the same hospital protocols as other surgeons. So, when you trust your feet to a Podiatric Surgeon, you can be sure they're in good hands.
Look around
Sign up for updates
Catch up on the latest industry news and foot health tips by signing up to our newsletter. You can also read up on all of our articles on our blog.
You need a helping hand with your project?
Thanks for signing up to our mailing list!
Oops, there was an error sending your message.
Please try again later
Please try again later
Opening hours
Monday 8am–5pm
Tuesday 7am–5pm
Wednesday 8am–7pm
Thursday 8am–7pm
Friday 8am–5pm
Disclaimer: The information in this website is not intended to be a substitute for professional Podiatric or medical advice. Always seek the advice of your Podiatrist or other qualified health practitioner before starting any new treatment or if you have any questions regarding a specific health condition.
Site by Helium Marketing